Childhood Abuse leads to Mental Health Issues Later in Life
Abstract
The information in this article is designed to reveal how childhood abuse may lead to mental health issues later in life. Not only is the number of reported child abuse cases increasing, but also many of these children meet the criteria for a “mental health illness” later in life. Although this is not the only cause for mental illness, it appears to be the most prominent one. Here I will examine the problem at hand and describe how the link between abuse and mental illness is formed.
The Problem: Abuse
In the year 2006 alone, there were a reported 905,000 cases of child abuse in the United States (Child Welfare Information Gateway, 2003). These numbers are constantly growing each year, and there may be more cases, which go unreported.
Although the definition of abuse may vary from person to person, it usually falls into one of the following categories:
- Sexual abuse
- Physical abuse (hitting, pushing, grabbing, ect.)
- Verbal abuse (constant yelling, swearing, mocking, insulting, intimidation)
- Neglect
- Witnessing abuse within the family
Any kind of abuse will leave a child with immediate physical or emotional trauma. However, the long-term mental effects are equally as bad.
The Problem: Mental Issue Development
Mental illnesses refer to a wide range of mental health conditions. Mayo Clinic defines a mental illness as “disorders that affect your mood, thinking, and behavior” (Mayo Clinic, 2012). Because these illnesses are so difficult to define, Psychiatrists and Psychologists use the Diagnostic and Statistical Manual of Mental Disorders (DSM) to classify an individual as having an illness or not.
However, some symptoms my not fall under any one specific category in the DSM. As a result, some cases of mental illnesses may go unreported. The following are a few of the most common mental illnesses that may be found in the DSM (Mayo clinic, 2012):
- Depression
- Anxiety
- Bipolar disorder
- Schizophrenia
- Eating disorders
- Addictive behavior
Symptoms of these illnesses may vary amongst each individual. If anything is out of the ordinary in a child’s behavior, then there may be cause for concern.
Now that we have seen both the cause (abuse) and effect (mental illnesses) separately, we can put them together to see how they relate.
A Case Study
In 2003, a study was conducted which evaluated 8,667 adult members of the Health Maintenance Organization (HMO). These individuals were asked to measure their exposure to family dysfunction[1] as a child. Afterwards, they completed a mental health assessment (“U.S. National Library of Medicine, 2003”).
It was found that 14% reported witnessing maternal violence, 20% experienced physical abuse, and 21% experienced sexual abuse. 34% reported more than one type of abuse. It was found that lower mental health scores correlated to higher numbers of abuse categories (“U.S. National Library of Medicine, 2003”).
As we can see, there is a strong relationship between experiencing/witnessing abuse as a child, and future mental issues that arise.
The Connection
The link between early abuse and future mental illness is extremely relevant when evaluating the statistics. In one long-term study, which followed abuse victims through their childhood until age 21, it was found that 80% were classified as having at least one psychiatric disorder (Child Welfare Information Gateway, 2008). This classification would follow the criteria set by the Diagnostic and Statistical Manual of Mental Disorders.
We first noticed a statistical connection between abuse and mental health impairment. Now we will examine how abuse causes mental issues from a physiological standpoint. In a study conducted, which evaluated the brain activity of abuse victims, there was a startling discovery of changes in and around the hippocampus (Szalavitz, 2012).
The hippocampus plays a crucial role in connecting emotions and senses to memory. During a child’s brain growth, the hippocampus wants to grow naturally, using emotions from the past, and linking them to memories. However, if a child has experienced negative emotions from abuse, there will be much higher levels of stress that the hippocampus must deal with (Welsh, 2012). This stress may cause the hippocampus to shrink, resulting in poor growth and development. All of this would then leave the abuse victim more susceptible to mental health issues such as depression or PTSD (Welsh, 2012).
To prove this, a Harvard study was conducted to evaluate the brains of abuse victims (Szalavitz, 2012). The breakdown was as follows:
- 200 adults aged 18-25 were recruited to recall their childhood memories of abuse
- 32% of these adults have experienced either depression or PTSD in their life
- Brain scans of the more significantly abused victims were evaluated
- On average, there was a 6% reduction in the hippocampus, and 4% reduction in the areas surrounding the hippocampus
Solution
Due to the severity and nature of this issue, finding a fast and simple solution is by no means easy. Ideally, we would want to stop the abuse before it happens. However, this is not always realistic. With the number of abuse victims increasing each year, it is difficult to pinpoint where they are happening. Therefore, we need to also issue a back-up solution after the violence has already taken place. This will either prevent or decrease the likelihood of the development of a mental health disorder. We can attempt to solve this issue in two different stages:
- Before the abuse can happen, or
- After the abuse has already occurred
Solution (#1)
The U.S. Department of Health and Human Services provides some excellent ways to prevent child abuse in households. A few of the solutions include (Child Welfare Information Gateway, 2008):
- Get to know your neighbors
- Keeping your neighborhood safe
- Reaching out to the children in your community
- Learning how to recognize and report signs of abuse
Much of this is common sense. Being aware and proactive is the best way to go about putting an end to abuse.
Solution (#2)
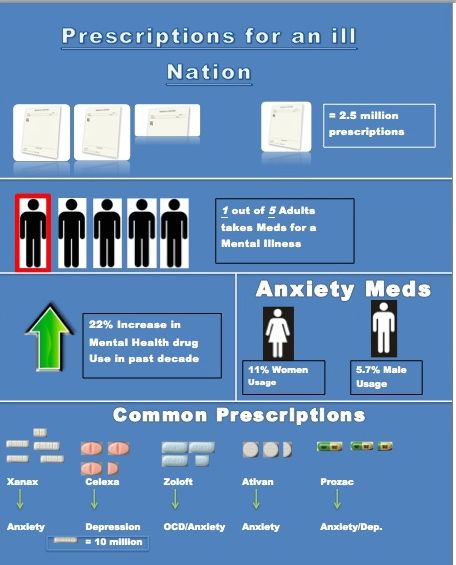
If abuse has already occurred, then we need to seek the second solution and make sure the child is not developing any mental disorders. The best possible way to go about this is to check for any type of unusual behavior. Is the child disconnecting from the outside world? Is he losing sleep, his appetite or drive to enjoy his life? It is important to recognize these cues early on. If these are discovered, then proper medical treatment (therapy, medications, ect.) may be necessary.
Conclusion
Not only is there a link between childhood abuse and mental health illness, but we also now have a biological way to prove it. Through case studies, statistics, and biology, we have seen that childhood abuse leaves its victims much more vulnerable to future mental illnesses.
There are approximately 4 million children evaluated for abuse or neglect each year (Szalavitz, 2012). With the evidence that has been presented here, it is likely that a large portion of these children will grow up to develop a mental issue if no action is taken. Realizing the cause of a problem is the first step in putting an end to it. Now that we have grasped the cause of mental illnesses, future work can be done to decrease or put and end to them.
[1] Family Dysfunction includes: sexual abuse, physical abuse, or witnessing maternal violence
References
Child Welfare Information Gateway. U.S. Department of Health and Human Services, Administration for Children and Families. (2008). Long-term consequences of child abuse and neglect. Retrieved from website: https://www.childwelfare.gov/pubs/factsheets/long_term_consequences.cfm
Child Welfare Information Gateway. U.S. Department of Health and Human Services, Administration for Children and Families. (2008). Preventing child abuse and neglect. Retrieved from website: https://www.childwelfare.gov/pubs/factsheets/preventingcan.cfm
Mayo Clinic. (2012, sept 15). Mental illness. Retrieved from http://www.mayoclinic.com/health/mental-illness/DS01104
Szalavitz, M. (2012, Feb 15). How child abuse primes the brain for future mental illness. Time: Health and Family, Retrieved from http://healthland.time.com/2012/02/15/how-child-abuse-primes-the-brain-for-future-mental-illness/
U.S. National Library of Medicine, National Institutes of Health. (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. Retrieved from website: http://www.ncbi.nlm.nih.gov/pubmed/12900308
Welsh, J. (2012, Feb 13). Child abuse leaves mark on brain. Retrieved from http://www.livescience.com/18453-child-abuse-brain.html